
Methadone: A Complete Guide to Treatment, Eligibility, and What to Expect
If you’re struggling with opioid use disorder in Delaware, methadone treatment can provide the stability you need to rebuild your life. This guide walks you through exactly how to access methadone treatment at our Delaware methadone clinic, what the process looks like from day one, and what you can realistically expect as you begin recovery.
What Is Methadone Treatment and How Does It Work?
Methadone is a long-acting opioid medication used to treat opioid use disorder. It works by reducing cravings and preventing withdrawal symptoms without producing the high associated with drugs like heroin, fentanyl, or prescription painkillers.
When someone is dependent on opioids, withdrawal symptoms and cravings can be so intense that willpower alone isn’t enough to prevent relapse. Methadone addresses this by stabilizing your body chemistry, allowing you to function normally throughout the day without needing to use street drugs.
Importantly, methadone also reduces the risk of fatal overdose, particularly for people who have overdosed before or are at high risk. It’s prescribed by our licensed medical providers and dispensed daily at our certified opioid treatment program.
Methadone isn’t a cure by itself. It’s what we call “one leg in the stool.” To be effective, it needs to be combined with counseling, mental health support, and help with other life challenges like housing, employment, or legal issues. At CORAS Wellness, we treat the whole person, not just the addiction.
How to Access Methadone Treatment in Delaware: Step-by-Step

Getting started with methadone treatment at our Delaware methadone clinic is more straightforward than many people expect. Here’s what the process actually looks like:
Step 1: Make Initial Contact
Call or walk into one of our Delaware locations offering MAT services. We have clinics in Dover, Newark, Harrington, and Millsboro. You don’t need a referral. You don’t need to explain yourself over the phone. Just show up or call to schedule an intake appointment.
Step 2: Initial Screening
When you arrive, you’ll take an instant drug screen and meet briefly with our staff to determine whether methadone treatment is appropriate for your situation. Not everyone who walks through the door needs methadone. Our medical providers screen each person individually.
For example, we recently had a young woman come in requesting methadone, but after reviewing her drug screen and meeting with our medical doctor, we determined that our Intensive Outpatient Program (IOP) and substance abuse counseling would be a better fit. Methadone is effective, but it’s a controlled substance and should only be used when medically appropriate.
Step 3: Intake and Orientation
If methadone is right for you, the intake phase begins. You’ll sign consent forms, receive a handbook explaining how our program works, and go through an orientation that covers rules, expectations, and what services are available to you.
Step 4: Comprehensive Assessment
This is the most time-intensive part of the process, but it’s essential. One of our counselors will conduct a full biopsychosocial assessment, examining not just your substance use but also:
– Physical health concerns
– Mental health conditions (depression, anxiety, bipolar disorder, etc.)
– Housing stability
– Legal or child welfare involvement
– Employment status
– Your recovery environment (Are you living with people who use drugs? Do you have support?)
This assessment drives your individualized treatment plan—we call them recovery plans at CORAS. It also determines what referrals you might need, whether that’s mental health care, case management, or help finding stable housing.
Step 5: Medical Evaluation and First Dose
On your first day, you’ll receive a full physical exam, lab work, and bloodwork. You’ll meet with our nursing staff and then with our medical director, Dr. Okechukwu Ernest Obua, who conducts a virtual evaluation with every new patient. He’ll determine your starting methadone dose based on your individual needs.
Over the first few weeks to a month, we’ll adjust your dose until we reach a level that keeps you comfortable and prevents cravings throughout the day.
Who Qualifies for Methadone Treatment in Delaware?
Methadone is appropriate for people with opioid use disorder who meet certain criteria. It’s particularly helpful for:
- People with long-term opioid dependence
- Individuals who have overdosed or are at high risk of overdose
- Those who have tried other forms of treatment without success
- People whose withdrawal symptoms are too severe to manage in outpatient counseling alone
Our medical providers make the final determination. You don’t need to be “sick enough” or prove you’ve hit rock bottom. But you do need to have a pattern of opioid use that warrants medication-assisted treatment.
What Does Methadone Treatment Cost in Delaware?
One of the most common questions we hear is: “How much is this going to cost?”
At our methadone clinic in, Delaware, most services are covered at no cost to you if you have:
- Medicaid (including Delaware First, Highmark, and Amerihealth)
- DSAM (state-funded coverage for uninsured individuals)
- Most commercial insurance plans through employers
If you have Medicaid or DSAM, you typically won’t receive a bill. If you do, bring it to our clinic and we’ll resolve it. Prescription co-pays through Medicaid may apply, but they’re usually minimal.
The screening, intake, assessment, counseling, and methadone dosing itself are all covered. Cost should not be a barrier to getting help.
What to Expect During Your First Week of Methadone Treatment
The first few weeks of treatment are about stabilization. Many of our patients describe it as a shift from chaos to structure.
When you’re in active addiction, life becomes consumed by the need to find money, avoid withdrawal, and keep using just to feel normal. We often hear people say they weren’t even using opiates to get high anymore, they had to use them just to get to baseline so they could function at all.
Methadone breaks that cycle. Our clinic opens at 5:00 a.m., so you can get your dose before work or other responsibilities. Once your dose is stable, you should feel comfortable throughout the day without cravings or withdrawal.
During the first week, you’ll:
- Come to our clinic five days a week for daily dosing (everyone gets Saturday and Sunday take-home doses to be with family)
- Begin meeting with your assigned counselor
- Start building a relationship with our medical and clinical staff
- Have your dose adjusted as needed based on how you’re feeling
Our goal is to find the right dose that eliminates cravings and withdrawal without sedating you or making you feel “high.”
Read more about what to expect here
Understanding Medication-Assisted Treatment (MAT) at Our Delaware Clinic
Methadone is one component of Medication-Assisted Treatment (MAT), the comprehensive approach we use at CORAS Wellness to treat opioid use disorder. Rather than medication alone, MAT integrates counseling, therapy, and case management to address every aspect of recovery.
Our MAT outpatient program combines:
- Medication (methadone, Suboxone, or Vivitrol)
- Counseling and therapy (individual sessions, group therapy, intensive outpatient programs)
- Case management (help with housing, employment, legal issues)
- Mental health treatment (for co-occurring conditions like depression or PTSD)
We have psychiatric nurse practitioners, licensed clinical social workers, and certified alcohol and drug counselors on staff. Our clinic serves patients in our MAT program, along with additional individuals in our other outpatient services.
If you have co-occurring mental health conditions like bipolar disorder, schizophrenia, or severe anxiety, treating only the opioid use disorder won’t be enough. Mental health and substance use are often intertwined, and both need to be addressed for long-term stability.
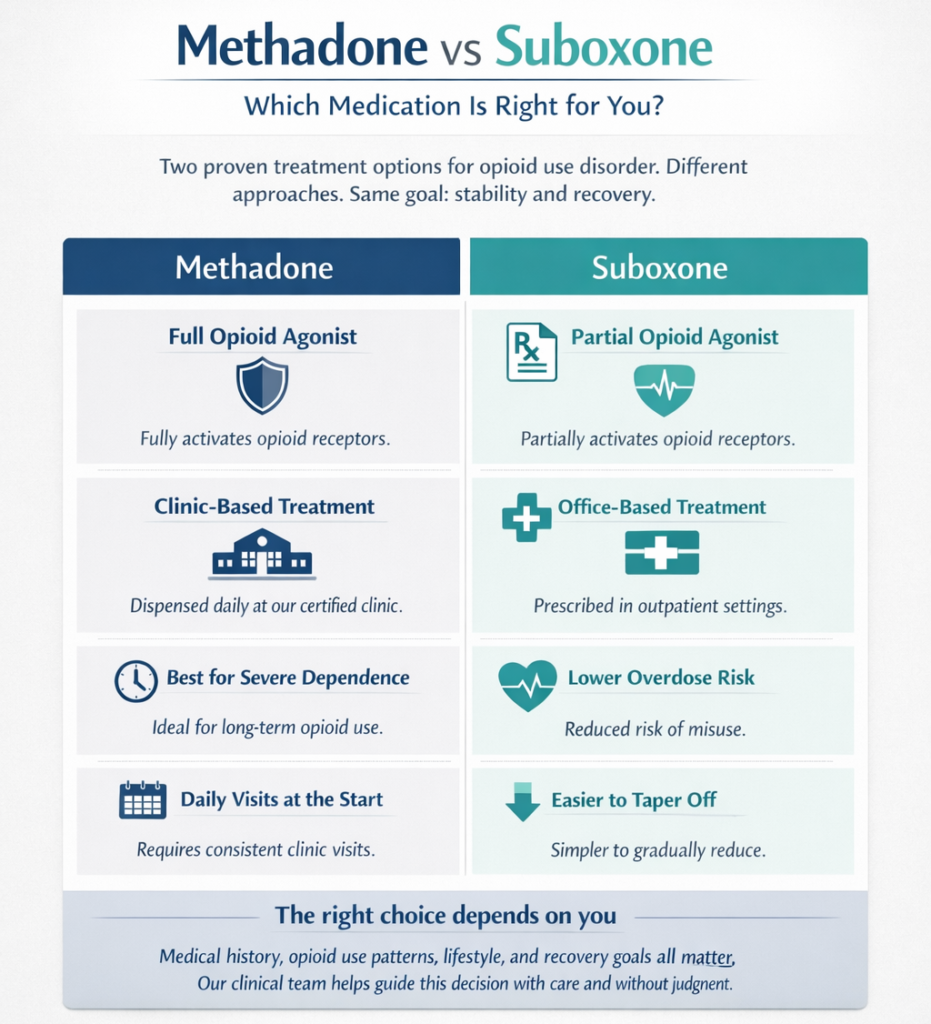
Methadone vs Suboxone: Which Medication Is Right for You?
Both methadone and Suboxone (buprenorphine) are FDA-approved medications for opioid use disorder, but they work slightly differently.
Methadone:
- Full opioid agonist
- Dispensed daily at our certified clinic (with take-home privileges earned over time)
- Longer track record for severe, long-term opioid dependence
- Requires daily visits initially
Suboxone:
- Partial opioid agonist
- Can be prescribed in outpatient settings
- Lower risk of overdose
- May be easier to taper off over time
Our medical providers will help determine which medication is best based on your history, severity of use, and personal circumstances. Some people do better on methadone; others prefer Suboxone. Neither is “better” in an absolute sense.
How Methadone Take-Home Privileges Work
One of the biggest changes in methadone treatment over the past few years is the expansion of take-home privileges. Historically, people had to come to clinics six or seven days a week for years before earning take-homes. That’s no longer the case.
At our clinic, the take-home schedule works like this:
- When you start: You come to the clinic five days a week. Everyone receives Saturday and Sunday doses to take home.
- After 30 days with a clean drug screen: You receive one week’s worth of take-home bottles and only need to visit once a week.
- After 60 days of clean screens: You receive two weeks’ worth of take-homes.
- After 90 days of clean screens: You receive a full month’s worth of take-home bottles and only visit once a month.
This structure has been positively received by our patients. It gives people more flexibility, reduces the disruption to work and family life, and serves as a strong motivator. If you relapse and test positive, you may return to more frequent dosing, but our goal is always to support your progress, not punish setbacks.
Take-home privileges also provide an additional layer of accountability. When you’re at home with your family and they see you’re doing well—going to the clinic only once a month—it can serve as a reminder of your progress and a reason to think twice before making an impulsive decision to use.
What Long-Term Success Looks Like in Our Delaware Methadone Program
There’s significant stigma around methadone, with some people viewing it as “trading one drug for another.” That misses the reality of what stability looks like for people in our program.
At our Dover clinic, approximately 70-75% of our methadone patients have earned take-home privileges, meaning they’re providing consistent clean drug screens and have found stability in their lives.
The patients who do best in our program typically:
- Attend counseling sessions consistently
- Participate in group therapy or our PHP/IOP program
- Address co-occurring mental health issues
- Change their “people, places, and things” outside of treatment
- Engage with community recovery support (like 12-step meetings, if that works for them)
Success isn’t just about staying clean. It’s about rebuilding a life.
I worked with a woman who entered our program while pregnant, struggling with crack cocaine, facing homelessness, and missing OB/GYN appointments. Through consistent treatment, mental health support, and a referral to a recovery house in southern Delaware, she got stable. She had a healthy baby, became the house manager at her recovery residence, and is approaching a year clean. Her boyfriend, who was also struggling in our program, saw her progress and went to inpatient drug rehab. He’s now earning take-home privileges and looking for work. When he comes to the clinic, we help him with diapers and other supplies from our baby shed.
That kind of transformation doesn’t happen because of methadone alone. It happens because methadone removes the chaos of active addiction and creates space for the harder work of recovery.
Common Fears and Misconceptions About Methadone
“Isn’t methadone just replacing one addiction with another?”
Methadone is a prescribed medication that allows you to function normally. It doesn’t produce a high when taken as directed. The goal is stability, not intoxication. Many people stay on methadone for years because it allows them to work, maintain relationships, and avoid the life-threatening risks of street opioids.
“I’ll have to go to the clinic every single day forever.”
Not true. With our updated take-home policies, you can earn monthly privileges within 90 days of clean screens. Many of our patients only visit the clinic once a month after they stabilize.
“I tried treatment before and it didn’t work.”
Recovery rarely follows a straight line. Many people need multiple attempts before finding what works. The structure, counseling, and support we provide now may be different from what you experienced before.
“I’m too old / too far gone / too broken.”
Age, history, and past failures don’t disqualify you from our program. Treatment is available regardless of where you’ve been or how many times you’ve tried before. Your destiny isn’t to be out here struggling.
How We Support Consistency: Counseling, Case Management, and Mental Health Services
Even with the best intentions, staying consistent with treatment can be difficult. Life happens. Mental health issues flare up. Housing becomes unstable. Family conflict arises.
We address these challenges through:
- Case management: Help with housing referrals, employment support, and navigating legal or child welfare systems
- Mental health services: On-site psychiatric providers for medication management and therapy
- Family involvement: With your consent, family members can participate in your care, report concerns, and stay informed about your progress
- Long-acting injectable medications: For people struggling with medication consistency, options like Vivitrol or long-acting antipsychotics can reduce the burden of daily pills
- Peer support and community: Coffee, refreshments, and a welcoming environment where our staff knows you by name
We understand that people with severe mental health conditions or unstable living situations may struggle more than others. Our goal is to meet you where you are and provide the support you need to stay engaged.
How Family Members Can Participate in Treatment
Family members often notice things that patients themselves don’t see. They live with the person and witness day-to-day changes in mood, energy, or behavior.
At CORAS, family involvement can take several forms:
- Releases of information: With your written consent, your counselor can speak with a parent, spouse, or other supportive person about your progress, medication side effects, and whether you’re attending appointments
- Family therapy sessions: Less common, but available if helpful
- Observational input: Family members can report symptoms or concerns, such as drowsiness, mood changes, or medication side effects
Many parents or spouses are primarily concerned about mental health medication compliance. They want to make sure that treatment isn’t just addressing opioid use, but also managing conditions like bipolar disorder, depression, or anxiety that may be driving the addiction.
Involving family requires balance. Some patients want autonomy in their sessions, and we respect that. But when family members are supportive and engaged, their input can be invaluable.
Frequently Asked Questions
How quickly can I start methadone treatment in Delaware?
You can often begin the same day you walk into our Dover, Newark, Harrington, or Millsboro clinic, depending on capacity and medical availability. The screening, intake, and first dose can all happen within the first visit.
What if I don’t have insurance or I’m homeless?
We accept DSAM, which covers uninsured individuals in Delaware at no cost. Homelessness is not a barrier to treatment. Our case managers can help connect you with recovery housing.
Can I work while receiving methadone treatment?
Yes. Our clinic opens at 5:00 a.m. to accommodate work schedules. As you earn take-home privileges, you’ll spend less time at the clinic and more time rebuilding your life.
What happens if I relapse while in the methadone program?
Relapse doesn’t mean you’re removed from our program. It may mean returning to more frequent dosing or increasing counseling support. Our goal is always to help you stabilize, not punish setbacks.
Does methadone work for alcohol or cocaine addiction?
Methadone is specifically for opioid use disorder. However, we offer substance abuse services for alcohol, cocaine, and other drugs. Medications like Vivitrol can also help reduce cravings for alcohol. A comprehensive assessment will determine the best treatment plan.
How long will I need to stay on methadone?
There’s no set timeline. Some people stay on methadone for months; others stay on it for years. The decision to taper off should be made collaboratively with our medical providers when you’re stable and ready.
Do you treat co-occurring mental health conditions?
Yes. We have psychiatric nurse practitioners and medical doctors on staff who can prescribe medications for depression, anxiety, bipolar disorder, and other mental health conditions. Treating both substance use and mental health together improves outcomes.
If You’re Unsure Whether Methadone Treatment Is Right for You
If you’re reading this and still on the fence, consider this: nothing changes if nothing changes.
You don’t have to be certain. You don’t have to have it all figured out. You just need the courage to take the first step.
Walk through our door. Have a cup of coffee. Meet with our doctor. See what we can do for you. Maybe it’s methadone. Maybe it’s counseling. Maybe it’s help with housing or mental health. But you won’t know until you try.
There’s all this help here—a warm cup of coffee, doctors, therapists, everyone who wants to help you. But you’ve got to take that first step.
Recovery requires two things: the courage to push through fear and self-doubt, and the determination to keep going when it gets difficult. It’s not easy. But on the other end is a whole life—peace, stability, relationships, a future.
If you’re ready to take that step, contact CORAS Wellness today. Treatment is available. Support is available. And you deserve a chance at something better.
